Somerset County, on Maryland’s Eastern Shore, has a nearly 16% COVID-19 positivity rate, the second highest in the state. According to the governor’s office, the majority of the county’s COVID-19 cases are linked to the prison in Westover, the state’s largest prison.
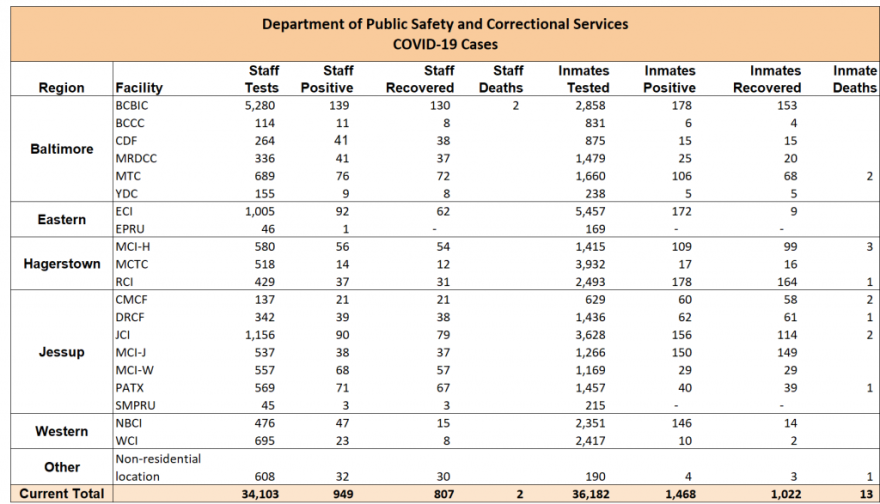
By the end of the third week of October, nine inmates and 45 staff members at Eastern Correctional Institution, or ECI, had tested positive for COVID-19 since the beginning of the pandemic.
Now, the state Department of Public Safety and Correctional Services says 163 inmates of the prison’s roughly 2,900 total population, as well as 30 of its roughly 700 staff members are currently infected, while another 62 staff members and 9 inmates have recovered.
Some inmates were recently forced to quarantine in the prison’s gym, said Jack Hughes, the Eastern Shore field representative for the American Federation of State, County and Municipal Employees, or AFSCME, the union that represents correctional officers and other staff at state prisons.
A former correctional officer at ECI, Hughes said the prison was short-staffed before the pandemic hit. Having so many staff out sick or on quarantine has exacerbated the problem.
Until recently, staff rotated between different parts of the prison complex to fill in for absent coworkers. Hughes said the prison ended that practice within the last couple of weeks out of concern the practice was spreading the virus.
“Public health in prisons is really equivalent to public health everywhere else,” said Leonard Rubenstein, who specializes in epidemiology at the Johns Hopkins Bloomberg School of Public Health. He said the more movement inmates and staff have inside prisons, the higher the likelihood of spread.
ECI is not the only state prison experiencing a spike in COVID-19 cases, according to data released by the Department of Public Safety and Correctional Services Monday. At North Branch Correctional Institution in Cumberland, 132 inmates and 32 staff have confirmed cases of COVID-19. At Jessup Correctional Institution, 42 inmates and 29 staff are currently infected. In fact, staff, inmates or both are infected at almost every state correctional facility.
Mark Vernarelli, spokesman for the Department of Public Safety and Correctional Services, declined an interview. In emails, he linked the spread of the virus inside prisons to the high rates of community spread seen statewide.
To prevent the virus from spreading, staff are required to wear masks, he said. The department also randomly tests 1,000 of its roughly 18,000 inmates each week.
“The Department is constantly testing, utilizing quarantine and isolation housing, and remaining nimble in modifying inmate movement to prevent and mitigate potential spread,” Vernarelli wrote.
However, Rubenstein, who recently co-authored a report about the risks of COVID-19 spreading in prisons, said the best way to mitigate a pandemic inside a prison is to reduce the prison population by releasing some of the inmates, giving those who remain a greater ability to social distance in the confined spaces of a prison.
Gov. Larry Hogan’s previous order authorizing the release of certain inmates did not go far enough, Rubenstein said. For example, it excluded many prisoners with chronic health conditions.
“When you do release people, you have to have a mechanism to protect them and the community,” Rubenstein said.
Upon release, inmates should be tested and may need to quarantine for two weeks, perhaps in hotels, to keep them from infecting their families and their communities.
“You want to make sure they have adequate support and housing and medical care and an income so they don't — are not induced to behave in ways that could spread the disease,” Rubenstein said. “You can prevent community spread if you do it in the right way.”






